Peter Saenz and Charles R. Goulding look at the progress of certified healthcare applications for 3D printing.
In 2021 the Food and Drug Administration (FDA) released a discussion paper and a request for comments to gather feedback that will be used to develop future policies and guidance regarding 3D printing at the point of care (POC). This is not the FDA’s first attempt to craft new guidance.
In 2017, the FDA released another technical considerations document that indicated the types of information that should accompany additive manufacturing (AM) medical device submissions. Also, in 2016, the FDA released technical considerations document outlining its initial thoughts on the technical considerations related to medical devices manufactured using additive manufacturing processes.
Though this guidance provides some clarity, the way regulation will translate to POC additive manufacturing is still opaque. Ultimately, the FDA wants to create a policy that assures that 3D printed medical devices are safe and effective, establishes the appropriate controls to ensure standards are met, and clarifies which entities are responsible for complying with the regulatory requirements at the POC.
The draft FDA framework does not yet address how the FDA will define the risks of different types of 3D printed medical devices. There needs to be a risk classification system that is based on how and where devices are manufactured at the POC. The legal liability for healthcare facilities and those engaged in AM needs to be established. These policies need to account for the FDA potentially not having the resources to oversee devices printed at healthcare facilities across the country. This ambiguity in policy is concerning because healthcare facilities are rapidly adopting 3D printing at the POC without clear guidance or oversight.
3D Printing has been around since the 1970s, but in 2019 the number of hospitals with centralized 3D printing facilities was only 113. From this vantage point, adoption seems to be occurring at a snail’s pace, but a different narrative unfolds after changing the time frame. From 2010 to 2019, the number of hospitals with centralized 3D printing facilities increased from 3 to 113.Even still, this does not tell the whole story because there are three primary models that hospitals can employ to facilitate adoption.
- Contracting with a 3D printing service bureau to obtain the appropriate 3D printing solution
- Hospitals like Mayo Clinic setting up their own centralized 3D printing facilities
- Hospitals bring in outside companies that set up and operate 3D printing facilities on-site
An example of model three is the Hospital for Special Surgery in New York City partnering with LimaCorporate to develop the ProMade Point of Care Center for Complex Orthopedic Solutions, which will be the first provider-based 3D design and printing facility for custom complex joint replacement solutions. When accounting for all three models, the number of hospitals adopting AM technology is much greater than the number of hospitals with centralized 3D-Printing capabilities.
Technological adoption is often slow until the needs of society dictate otherwise. mRNA vaccine technology coupled with the COVID-19 pandemic is an exemplary case in point of this phenomenon, but the pandemic was also the impetus for widespread 3D printing adoption. The surge in demand for personal protective equipment and the supply chain challenges of the pandemic provided the perfect conditions necessary for society to dive headlong into 3D printed personal protective equipment (PPE). Many hospitals began to print their own PPE while also receiving 3D-printed PPE donations from universities, hobbyists, and the public at large.
3D printed PPE became so prolific that the FDA released multiple guidance publications. The most recent publication was a Q&A regarding the 3D Printing of various medical PPE. The main takeaway of the announcement was that 3D-printed PPE might provide a physical barrier, but it may not provide the fluid barrier and air filtration required to prevent the spread of disease. This is due to 3D-printed products being essentially hundreds to thousands of layers of plastic stacked on top of each other. These layers do not create a perfect seal and therefore are porous.
The FDA’s Center for Devices and Radiological Health regulates 3D-printed devices based on risk. There are three regulatory class levels, with increasing levels of oversight based on the risk they pose to patients. The FDA regulates the overall manufacturing processes and medical devices but not the actual 3D printers. Then there are the FDA’s Center for Drug Evaluation branch and its Biological Evaluation and Research branch, which will probably play a role in regulating the Printing of pharmaceuticals and bioprinting, but these branches have yet to release definitive guidance.
Even with the advent of mass printing of PPE, most FDA-reviewed medical products developed utilizing AM have been orthopedic implants, with more than 100 reviewed. The FDA’s current medical device regulatory framework applies to all medical devices regardless of how they are manufactured. This creates ambiguity for both medical device manufacturers and hospitals. Questions that need to be addressed are whether products made at the point of care POC must meet the exact requirements of products produced at a conventional medical device manufacturing facility. This will be a crucial decision because hospitals are not designed to be manufacturing facilities.
Mandating absolute compliance will likely require more significant investments in infrastructure and ultimately curtail adoption. This doesn’t mean the bar should be set lower for 3D printed devices at the POC. The same standards should be met, but the regulation should allow hospitals flexibility in how they secure the bar. Furthermore, it would be eminently profitable to draw on the collective intelligence of the clinical and medical device communities to identify risks associated with additive manufacturing in their respective settings.
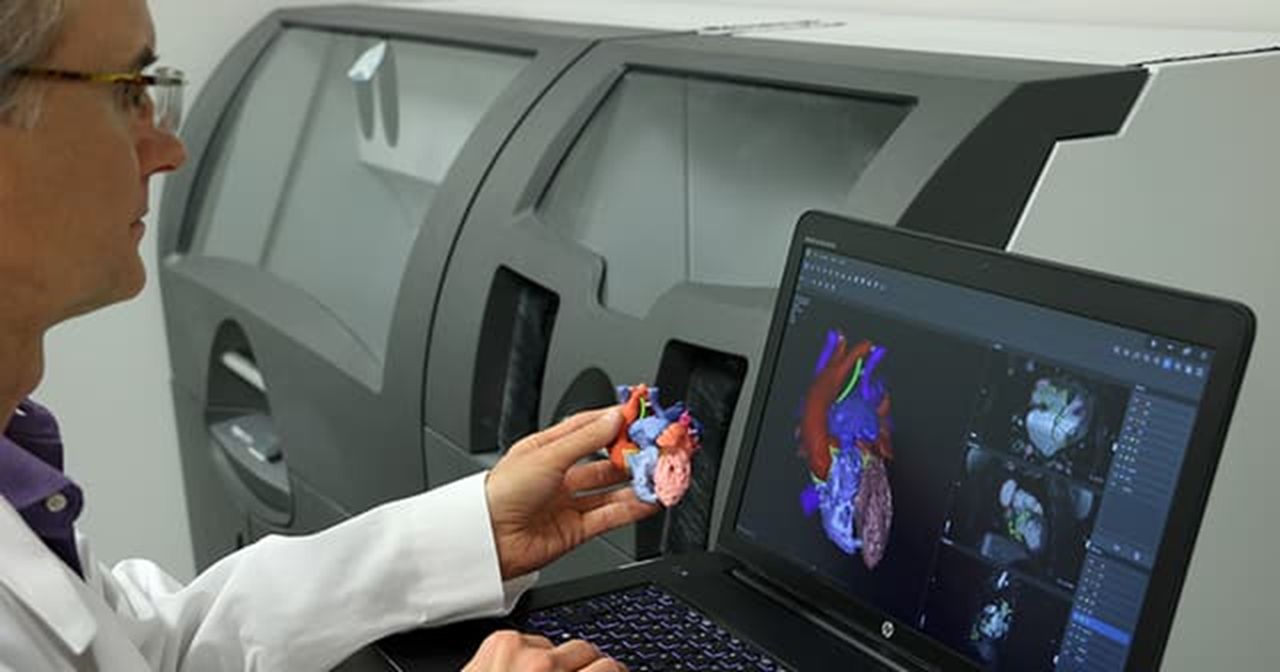
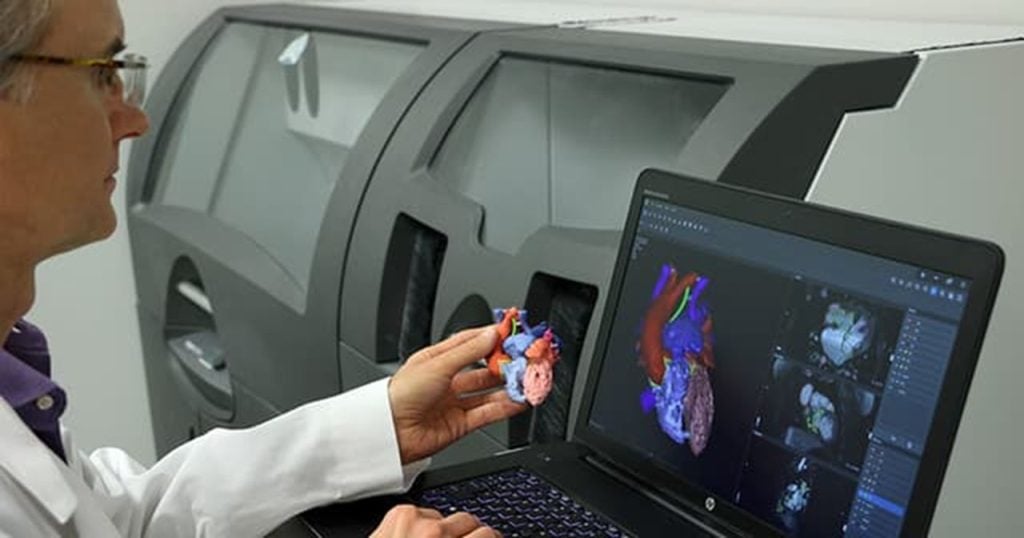
When the governing constraint of medical advancement is the promise of “primum non nocere,” Latin for “first, do no harm” of the Hippocratic Oath, a hierarchy of what medical devices should be manufactured first using 3D printing technology emerges. An argument can be made that the 3D printing of anatomical models is the lowest-hanging fruit when developing safe technology that reduces cost and improves the quality of care. Surgeons use these highly accurate and detailed anatomical models to prepare for complex procedures, thus reducing the time and cost of performing surgeries while improving clinical outcomes.
The technology aims to make highly skilled surgeons even more efficient and effective. Even if the model was inaccurate, surgeons should be able to self-correct when performing the surgery live. The worst-case scenario is that the surgeon wastes time training on an inaccurate model and hospital resources to produce the model. The 3D Printing of medical equipment, implants, and prosthetics can reduce costs and tremendously improve the quality of care. Still, since these products often directly interact with the patient or the clinician, there is a greater possibility of causing physical harm.
Another regulatory challenge for 3D printing at the POC is that most insurance carriers do not reimburse the use of additive manufacturing in patient care. Without category one Current Procedural Terminology (CPT) codes developed by the American Medical Association, healthcare facilities will be responsible for covering the cost of adopting this technology.
More manufacturers and healthcare networks will enter the space once the appropriate CPT codes are developed, and they know that the Centers for Medicare & Medicaid Services will reimburse codes for medical devices 3D printed at the POC. In addition to reimbursement, tax benefits are also available for manufacturers and healthcare networks.
Conclusion
The future of healthcare is bright, and the ways that additive manufacturing can be implemented abound. Still, a tremendous amount of work lies ahead in developing the regulatory framework of additive manufacturing at the point of care. The importance of this work cannot be understated since mistakes will result in deleterious outcomes and a lack of confidence that will hamstring the adoption of this promising technology.